COPD
Chronic Obstructive Pulmonary Disease (COPD)
What is COPD? Imagine your lungs like a set of balloons and tubes.
Normally, when you breathe in, air travels easily through the tubes (called airways) into tiny air sacs (like the balloons) in your lungs. These air sacs are stretchy and help get oxygen into your blood and carbon dioxide out.
With COPD (Chronic Obstructive Pulmonary Disease), this process doesn't work as well. It's a long-term lung disease that makes it hard to breathe. Think of it as having two main problems that often happen together:
The tubes get damaged and inflamed (like in Chronic Bronchitis):
The airways become swollen and irritated.
They might produce a lot of thick mucus (phlegm) that clogs them up.
This makes the "tubes" narrower and harder for air to flow through. People often develop a persistent cough trying to clear this mucus.
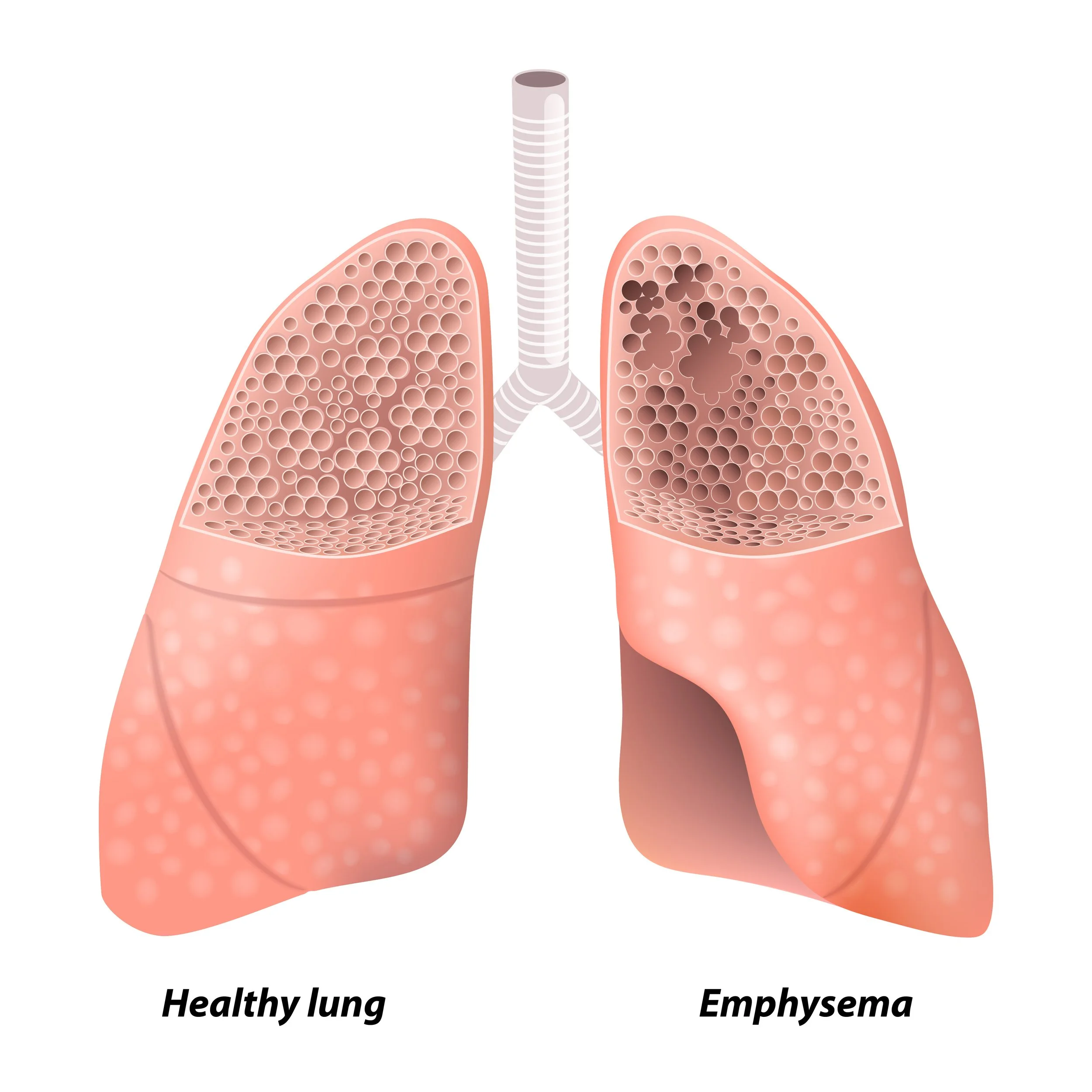
The air sacs get damaged (like in Emphysema):
The tiny air sacs lose their stretchiness, like an old rubber band.
The walls between some air sacs can get destroyed, creating fewer, larger sacs instead of many tiny ones.
This makes it harder for your lungs to take in oxygen and get rid of carbon dioxide. Old air can get trapped, making it difficult to get fresh air in.
In short: COPD means your lungs have trouble moving air in and out easily, so you don't get enough oxygen, and it's harder to get rid of waste air (carbon dioxide). This often leads to feeling breathless, especially with activity, a chronic cough, and wheezing.
How is COPD Treated? There's no cure, but treatment can really help manage it.
The main goals of treatment are to:
Make breathing easier.
Reduce how often you have bad flare-ups (when symptoms get suddenly worse).
Help you stay active and improve your quality of life.
Slow down the disease.
Here are the common ways COPD is treated:
Stop Smoking (This is #1!): If smoking is the cause (which it usually is), quitting is the most important thing you can do to stop further lung damage and prevent COPD from getting worse faster.
Medications (often using inhalers):
Bronchodilators: These are medicines that help relax and open up your airways, making it easier to breathe. Some are "rescue" inhalers for quick relief, and others are long-acting for daily use to keep airways open.
Steroids (inhaled): These can help reduce swelling and inflammation in your airways. They are often used regularly to prevent flare-ups. Sometimes, steroid pills are used for a short time during a bad flare-up.
Combination Inhalers: Many people use inhalers that combine a bronchodilator and a steroid.
Antibiotics: If you get a lung infection (which can make COPD much worse), your doctor will prescribe antibiotics.
Pulmonary Rehabilitation: This is a special program that can make a big difference. It usually includes:
Exercise training: Safely learning how to exercise to improve your breathing, strength, and stamina.
Education: Learning more about COPD, how to manage it, how to use your medications correctly, and breathing techniques.
Support: Getting advice on nutrition and emotional support.
Oxygen Therapy: If your COPD is severe and your blood oxygen levels are too low, your doctor might prescribe oxygen. You breathe it in through a nasal cannula (small tubes in your nose) or a mask. This can help you feel less breathless and protect your organs.
Lifestyle Changes:
Avoid lung irritants: Stay away from smoke, dust, fumes, and air pollution as much as possible.
Get vaccinated: Flu shots, pneumonia shots, and COVID-19 vaccines are very important to prevent infections that can worsen COPD.
Healthy diet and hydration: Good nutrition helps your body stay strong, and drinking enough water can help keep mucus thinner.
Learn breathing techniques: Special ways to breathe can help you manage shortness of breath.
Surgery (in rare, specific cases): For a small number of people with certain types of severe emphysema, surgery might be an option. This could involve removing damaged parts of the lung or, in very severe cases, a lung transplant.
Living with COPD involves working closely with your doctor to find the best treatment plan for you and making lifestyle changes to manage your symptoms and stay as healthy as possible.